A cluster randomised, parallel-group, 5-year trial of coordinated, co-produced care to reduce the excess mortality of patients with severe mental illness by improving the treatment of their comorbid physical conditions.
Background
People with severe mental illness (SMI) comprise about 2% of the Danish population and they die 10-20 years earlier than people without SMI [1]. In Region Zealand and Central Denmark Region, the 10-year mortality of patients aged 18-65 admitted to a psychiatric department during the preceding 5 years is 18.1%, while it is 4.3% in the rest of the population. Most of this excess mortality stems from physical diseases [2], which are underdiagnosed and under-treated [3]. These patients are treated across sector borders and coordinated care between general practice, municipalities and hospital psychiatry is considered imperative. Different initiatives using integrated care models designed outside general practice have been tested but with disappointing results and with difficulties in engaging both patients and general practice [4].
Objectives
The SOFIA project aims is to reduce all-cause mortality in people with SMI.
- The project will develop, execute, and rigorously test in a randomised controlled trial (RCT) an intervention consisting of a coordinated care plan supported by an integrated information and communication technology (ICT) care platform. This care model targets challenges with insufficient care in this vulnerable group, in particular underdiagnosis and undertreatment of comorbid physical conditions.
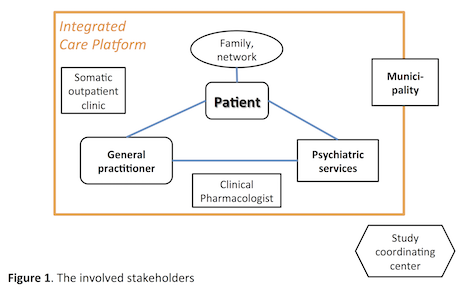
- The intervention will be developed by combining state-of-the-art evidence-based clinical, social and technological knowledge with the perspectives of all involved parties in a participatory co-design process (Figure 1).
The intervention
The main focus of the proposed intervention will be on improving the detection and pharmacological treatment of physical diseases in patients with SMI through a mutually committed and efficient cross-sectorial collaborative team. The team which includes clinical pharmacologists, social workers and psychiatrists who support the primary care professionals responsible for the sustained medical care of SMI patients. Alongside, viable lifestyle changes will be implemented. Harmful drug effects and interactions will be minimised through individualised advice from the clinical pharmacologist. A general practice nurse will be appointed to take responsibility for the coordinated care plan of the individual patients.
Eligible patients will be contacted from general practice and invited to participate. An individual treatment plan with realistic and individual goal-setting to engage patients in their treatment, will be worked out for each patient and approved by all stakeholders. Further consolidation of the individual care plan is sought by involving the patient’s family and network. The plan will follow the patient across sector borders, and the ICT care platform will provide up-to-date information flow between all stakeholders. Throughout the intervention period regular teaching sessions for patients and professionals and cross-sectorial workshops will be conducted to support the implementation and sustainability of the coordinated care model.
The SOFIA project puts focus on:
- SOcial clinical space – The ”patient part” of the consultation.
- FInd any underdiagnosed or undertreated somatic diseases
- Agree on individual care plan – Plan para-clinical tests if relevant. Plan for further checkups if relevant.
Technological solutions
An ICT care platform will be developed to support two fundamental purposes:
- effective communication and collaboration between all stakeholders and
- strengthening patients’ participation and adherence to effective treatment of comorbid physical diseases.
The work with the first purpose will be based on prior research in computer supported cooperative work (CSCW) for healthcare coordination [5]. For the second purpose the approach of Personal Health Technology [6] will be applied to develop a patient platform as a basis for patient involvement and to provide essential data streams for disease monitoring, analysis, and prediction. In combination, (1) and (2) will provide an ICT care platform which actively engages both the professional care team and the patient in monitoring and treatment of diseases. This allows for early intervention based on triggers and warning signs enabling a proactive care model based on shared decision-making.
References
- Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol. 2014;10:425-448.
- Lawrence D, Hancock KJ, Kisely S. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ. 2013;346:f2539.
- De Hert M, Cohen D, Bobes J, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry. Jun 2011;10(2):138-151.
- Speyer H, Christian Brix Norgaard H, Birk M, al. e. The CHANGE trial. World Psychiatry. Jun 2016;15(2):155-165.
- Bardram JE, Hansen TR. Context-Based Workplace Awareness. Computer Supported Cooperative Work (CSCW). 2010;19(2):105-138.
- Bardram JE, Frost M. The Personal Health Technology Design Space. IEEE Pervasive Computing. 2016;15(2):70-78.