With an increasingly older population and a shrinking work force, there is a need to streamline the available resources. By using wearable sensors to monitor a patient’s condition, the resources of medical staff can be used more effectively on more demanding tasks than simple surveillance.
Find the PhD here
Background
By the year 2040 it is expected that there will be twice as many older people (over 80), while the work force (under 65) is expected to become almost half of what it is now due to factors such as declining birth rates. The challenges that rise from this will force medical staff to spend less time on trivial yet vital tasks such as surveillance. Fortunately, much has happened in the development of wearable sensors over the past few years, making it possible to create devices that can measure vital signs and unobtrusive to the wearer.
Project Objectives
The main objective of the project is to investigate the benefits of continuous vital sign measurements in critically ill patients. The measurements focus on vital signs that can be monitored non-invasively, such as pulse, temperature, blood pressure and oxygen saturation. The long-term aim is also to monitor persons with chronic diseases in the private sphere.
The first phase focuses on existing measurements for patients with very diverse conditions at intensive care unit (ICU) at Bispebjerg Hospital. Vital sign measurements are combined with automatically extracted entries from the patient’s electronic health records. These different data are combined to create an overview of the patient’s physiological condition throughout an admission.

Figure 1: Raw vital sign measurements of a patient (top) along with their corresponding physiological condition (bottom) at any given time. The higher the physiological condition score, the worse is the patient’s condition. Orange color indicates that data is missing and physiological condition cannot be estimated.
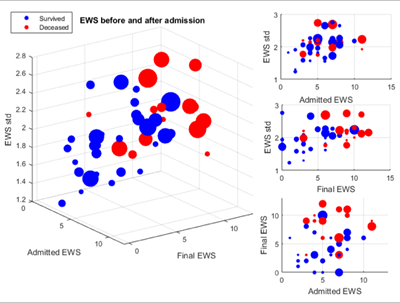
Figure 2: Physiological condition assessed before, during and after admission. Bubble size indicates length of stay. The condition of surviving patients (blue) fluctuates less during admission than it does for deceased patients.
The second phase is conducted at Zealand University Hospital, Roskilde and narrows the patient group down to focusing on stroke patients where vital signs are monitored less frequently. The focus here is to determine early markers for positive outcome after stroke.
One third of stroke patients have unrecognized diabetes mellitus (DM). The final project phase aims at automatically detecting which stroke patients are diagnosed with DM. If the two patient groups are distinguishable without using the information about whether they have the disease, it becomes possible to also identify unrecognized DM patients.
References
[1] Vilic, Adnan, et al. "Simplifying EHR Overview of Critically Ill Patients Through Vital Signs Monitoring." IEEE Journal of Biomedical and Health Informatics (2016).
[2] Vilic, Adnan, et al. "Visualizing patient journals by combining vital signs monitoring and natural language processing." Engineering in Medicine and Biology Society (EMBC), 2016 IEEE 38th Annual International Conference of the. IEEE, 2016.
[3] Vilic, Adnan, et al. "Queue-Based Modelling and Detection of Parameters Involved in Stroke Outcome" Engineering in Medicine and Biology Society (EMBC), 2017 IEEE 39th Annual International Conference of the. IEEE, 2017.
[4] Vilic, Adnan, et al. " Automatic Identification of Diabetes Based on Vital Signs and Medical History in Post-Stroke Patients" Engineering in Medicine and Biology Society (EMBC), 2017 IEEE 39th Annual International Conference of the. IEEE, 2017